


How would you feel if you or any of your loved ones needed an immediate blood transfusion and the doctor told you with a gloomy face that it could not happen because of a shortage of blood in the hospital bank?
Ganymede may not be a recognized name, but its work is gaining the right kind of recognition for one bold reason: it is working to create artificial blood in the lab as a way of creating an alternative to address the global shortage that hospitals and patients have suffered from for decades.
Since 1818, when James Blundell performed the first successful human blood transfusion to treat postpartum hemorrhage, modern medicine has continued to bank on a frail system to keep patients alive—human blood donation. This frail system is responsible for a lot of things.
Cancer treatment, illnesses, complications during childbirth, trauma aftercare, and surgeries. Donations can become irregular, facilities may store blood improperly or let it expire before use, and demand keeps rising. These are real problems that Ganymede is attempting to solve.
Ganymede is building artificial blood, a lab-grown alternative that aims to supplement and eventually meet the ever-growing demand for blood. Since solely relying on donors has proven to be ineffective on a large scale, Ganymede is looking to use bioengineering to create blood products in controlled laboratory environments.
Any assumptions about immortality or physical enhancement are far-fetched. Ganymede focuses on something far more practical: ensuring that hospitals always have safe, compatible blood whenever shortages occur.
As experts have noted, blood shortages are a problem for hospitals everywhere in the world. As people grow older, they require more transfusions but donation of blood has reduced in many places. There’s a number of reasons why this happens ranging from emergencies, pandemics, and sometimes death. All of these further disrupt the systems. While their scarcity may not happen constantly, they still face shortages of specific blood types.
These issues make blood one of the most essential yet difficult biological resources to access. Ganymede is trying to answer a complex question. What if labs could manufacture blood on demand? Instead of relying strictly on donations, this could prevent shortages before they happen.
When you hear of artificial blood, what comes to mind? Artificial blood isn’t a replica of what runs through our veins neither is it a replacement for it. So what is artificial blood? It is an engineered, temporary red blood cell substitute. Designed to transport oxygen through the body, primarily during emergencies and other medical procedures.
It is made to be stable, sterile, and compatible for all blood groups, reducing the stress that comes with looking for an exact blood type.
Ganymede’s work is centered on bioengineering. The company uses controlled laboratory processes to “grow” blood components under precise conditions.
This method has several advantages including:
Ganymede’s research focuses on enhancing these advantages so that artificial blood behaves as predicted inside the human body without causing complications.
One of the biggest obstacles artificial blood creation is facing is being accepted clinically. Blood is different from all the other medical products around; it interacts with human physiology. Because of this reason, artificial blood clinical trials are essential.
Ganymede is working to show that its blood products can be trusted for use. The trial carried out will test for its effectiveness, how this blood circulates, how it remains functional, and especially how the body responds to it.
If artificial blood ends up being accepted after successful trial tests, it could potentially change how hospitals work with blood. They don’t need to depend on donation and blood banks alone, there will be an alternative option to ensure shortages don’t happen again. Emergency wards will be well equipped to handle any critical condition, hospitals in rural areas will have access to blood and save lives without going through complex procedures.
For doctors and healthcare professionals, there’ll be less delays, less risks, and fewer canceled appointments. For patients, the good news is faster treatment and fewer issues regarding blood compatibility.
A merger of regenerative medicine and transfusion science is what suits Ganymede best. Given its work in addressing the biggest problem relating to one of the most universally used medical resources. This complements the growing trend in medicine, where labs now produce biological resources instead of collecting them from donors with syringes. The vision here is to ensure a reliable medical system that can function independently outside the unpredictable human supply.
Artificial blood is not yet accepted as an alternative for donated blood clinically. There are factors like certain immune functions, clotting factors, and specialized components that can’t function without the use of donor-derived products. But Ganymede’s work represents a meaningful shift toward reducing dependency where it matters most: oxygen delivery in critical care.
As researchers continue to carry out clinical trials and improve production methods, things may change. If the trials succeed and gain acceptance, Ganymede’s work could become the benchmark for the beginning of a new era in healthcare—one where labs can produce blood with the same reliability as modern pharmaceuticals by merging transfusion with lab-grown manufacturing. An alternative to solve the problem that donation can’t handle on its own.
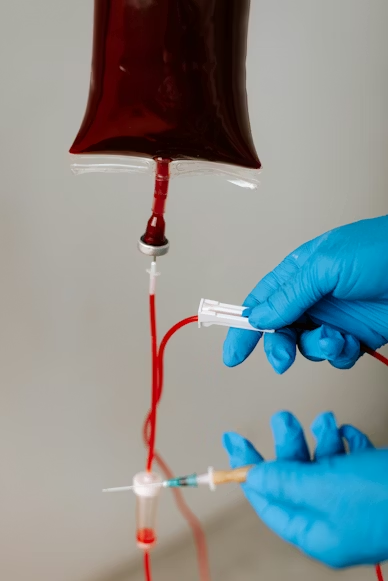
Image: Unsplash
Blood donation depends on people that are available, willing and most importantly, eligible to give blood. Even in countries that have cultures that encourage blood donation, willingly or monetary, they still fall short in some emergency cases, and also during pandemics or conflicts. Also, blood expires very quickly. For red blood cells, it can last for a couple of weeks and platelets last only for a few days.
Medical teams must store blood under careful temperature control to prevent bacterial growth and ensure it is safe for transfusion.
Regardless, demand for blood keeps rising in every part of the world. For instance, in the United States, every two seconds, someone needs blood. Aging populations, difficult surgeries, trauma care, and cancer treatments are some of the cases that are heavily dependent on blood transfusions if they are to work. The downside of what this leads to is a frail system where hospitals operate on the brink of collapse.
And because of this imbalance in the medical field, Ganymede is now in existence to fix this problem that has become structural.
The trials for artificial blood are currently carrying out a test for hemoglobin-based oxygen carriers (HBOCs) and lab-grown red blood cells as a solution to the problems that come with blood shortages. Recent studies done in Japan showed promising safety results in early-phase human trials with mild side effects like fever and rash that were quickly resolved.
Key trials included injecting hemoglobin vesicles for oxygen transport and transfusing stem-cell-derived, lab-grown red cells.
In 2022, researchers at Nara Medical University began trials with HbVs, which contain hemoglobin enclosed in a lipid shell. Twelve people volunteered for the study, and after researchers carried out tests, the results showed it to be a safe alternative to real blood cells. The team has made plans to increase doses from 100mL to 400mL in future phases.
In November 2022, the NHS Blood and Transplant announced they were attempting the first-ever clinical trial of laboratory-grown red blood cells transfused into another person. It was carried out by testing blood grown from donor stem cells to see if it’ll be able to last longer than the standard donor blood.
This is a universal synthetic blood product that is being developed to be preserved in the form of powder and redesigned with water. ErythroMer has shown success in animal trials and its next phase is to carry out human trial tests, designed to function as a short-term option for battlefield or emergency use.
This is an older, fully hemoglobin-based oxygen carrier (HBOC) that got to Phase III trials for treating trauma patients.
These are oxygen-carrying emulsions that remain motionless.
Researchers hope that by 2030, they’ll be able to achieve routine clinical use for certain products that can be used irrespective of patient blood type.
Ganymede is a key part of a larger movement that’s attempting to change how hospitals get its most critical service by providing an alternative. Just as lab-grown organs and AI-drugs are becoming trendsetters when it comes to treatment, synthetic blood is looking to do the same thing with self-sustaining medical systems.
Its work is pointing to a future where life-saving resources are not limited by any factor. Instead, they’re readily available as soon as demand is made.
Wrapping up, artificial blood isn’t looking to replace donors anytime soon. Its creation is to address the chronic scarcity that hospitals face all over the world. In that sense, what Ganymede is doing isn’t just “creating blood”. They’re providing solutions to help the medical sector and save more lives.